Making sense of the research on COVID-19 and masks
Benjamin W. Abbott1, Mitchell Greenhalgh1, S. Isaac St. Clair1, Jonas Bush2
1. Brigham Young University, Environmental Science; 2. Brigham Young University, Genetics, Genomics & Biotechnology
The interpretation and content of this report are those of the authors. (Published on 19 July 2020. Last updated on 21 August 2020). For the PDF version of this report, click here.
Scientific evidence can be difficult to interpret under the best of circumstances. During a global pandemic (and election year), it is no surprise that there is public confusion about what measures can effectively protect families and communities from COVID-19. Because the scientific and medical understanding of this disease is advancing so rapidly, we decided to put together a plain-language summary of the science on face coverings—a.k.a. masks. As lifelong residents of Utah County and scientists, we felt a responsibility to respond to the technical questions asked by friends and family. We did not receive any funding to carry out this work, nor do we plan on seeking financial support on this topic (our BYU lab mainly researches water and air pollution: benabbott.byu.edu).

Our four-person team compiled and read over 115 scientific studies on COVID-19. These studies were done by independent groups from all around the U.S. and the world. In the paragraphs below, we have done our best to accurately reflect the scientific evidence, pointing out where it is solid and where there is still uncertainty. There are four sections, with increasing levels of detail: 1. An executive summary, 2. A list of common questions, 3. A deep dive, and 4. FAQs about the study. We hope this summary is useful to you as you decide what is best for your family and as our community decides how best to face this threat together.
Executive summary:
- In the first few months of the pandemic, there was scientific uncertainty about the usefulness of public masking. Conflicting guidance was given by several official sources1–4.
- There is now convincing evidence from multiple controlled experiments5–7 and field observations8–14 that wearing masks reduces the transmission of COVID-19 for healthcare workers and the public. Most of this evidence is COVID-19 specific and has emerged in the past few months1,8,15,16.
- Masks prevent infected people from spreading the virus to others by trapping the respiratory droplets (tiny moisture particles) that are produced when we cough, speak, and breathe11,17,18. Cloth masks can stop 90% or more of the dispersal of droplets carrying the virus6,17,19,20. There is some evidence that cloth masks also protect the wearer from infection8,9, though this is less certain.
- Masks are highly safe, with only minor and uncommon side effects1,21,22. In addition to many medical studies, public masking has been proven safe among children, adults, and the elderly in cultures where this practice has long been common11,23. However, some individuals should not wear masks, such as those with severely compromised respiratory systems24 and individuals who cannot remove or adjust their own masks (children under 2 and people with severe disabilities)18.
- Researchers from hospitals, universities, the private sector, and government agencies have concluded that masks could be one of the most powerful and cost-effective tools to stop COVID-19 and accelerate the economic recovery1,5,10,11,16,23,25. There is universal agreement, however, that masking alone will not be enough to stop the pandemic. Masking is most effective when combined with physical distancing, frequent handwashing, rapid testing, and coordinated contact tracing1,8,26.
Common Questions:
What is COVID-19?
Coronavirus disease 2019 (COVID-19) is caused by a respiratory virus named “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2). It is in the same family as the virus that caused the SARS outbreak of 2003, and both of the viruses appear to have originally come from bats27,28 . The “severe” part of the virus’s name comes from its extreme contagiousness and serious complications. Thankfully, most people who have COVID-19 only experience flu-like symptoms such as fever, cough, difficulty breathing, and fatigue. However, COVID-19 is much more contagious than the flu, and it has a much higher death rate: 0.3 to 5.7% based on the most reliable estimates29–34 . For reference, the common flu has a death rate of 0.1%. Serious COVID-19 complications include damage to the lungs, liver, and heart, permanent loss of taste and smell, blood clots, stroke, and death31 . The rate of complications including death is much higher in individuals with preexisting conditions, particularly the elderly and those with cardiovascular disease, diabetes, respiratory conditions, high blood pressure, cancer, an organ transplant, sickle cell disease, immune disorders, and those living in areas with more air pollution33,35,36 .
How is COVID-19 transmitted?
While much is still being learned about this disease, it appears that the main way the virus is spread is through small droplets of moisture that are produced when a person exhales, talks, coughs, or sneezes5,34,37. These tiny droplets can travel many feet through the air and linger in the air or on surfaces for several minutes to hours after the infected person has left the area17,19,35,38,39. The virus can enter a new person’s body directly by being breathed in or landing in the eyes, nose, or other mucus membranes40–42. The virus can also spread indirectly through objects and surfaces.
After infection, most people experience an incubation period where there are no symptoms—typically lasting 5 days, but sometimes lasting 15 days1,5,43. Infected individuals are most contagious during the day before first symptoms and in the few days after onset, meaning that people who feel completely healthy can spread the virus to loved ones and strangers10,37,44. Up to one in three COVID-19 carriers show no symptoms at all (asymptomatic)12,45, though they can still spread the virus1,4,46. It is estimated that half of all transmissions occur from individuals not showing symptoms1,47. We have compiled information on the pathology of COVID-19 in children, adolescents, and young adults in a new report that is freely accessible here48.
Are masks effective for individuals and communities?
There is clear evidence that face coverings reduce the spray of droplets produced during speaking, coughing, and sneezing6,17,19,49–52. This is why masks have long been recommended for individuals with respiratory infections7,7,40,53–55. Furthermore, home-made cloth masks are similar in effectiveness to surgical masks in diffusing the “jets” of droplets that could spread COVID-19 (for details on mask types, see Figure 1 and the “deep dive”)6,19. For example, one of the most definitive studies on viruses and face masks found a 90% reduction in influenza viruses after breathing through a mask and a complete removal of coronaviruses50. However, not all face coverings are equally effective. Multi-layer synthetic and cotton masks provide the most filtration, while bandanas and fleeces (neck gaiters) provide very little or no protection6,20. Because only fitted respirators (the finest-meshed masks) provide reliable protection from external droplets and viral particles41,53,56, public masking works through “source control,”15 where “my mask protects you, and your mask protects me.”50
While it is always difficult to establish cause and effect at the community level, there is now strong evidence that public masking can slow or even stop the spread COVID-19 in states and countries4,7,11,13,16,44,57. One of the most conclusive studies on the subject compared the effectiveness of universal masking in the health-care system of Massachusetts8. This large study involved 75,000 participants, including healthcare workers and patients. Of all the public health interventions, universal masking appears to be the most associated with stopping the exponential growth of COVID-19 cases, first flattening and then decreasing the infection rate8. Another study from Missouri demonstrated the effectiveness of universal masking in commercial settings9. Two hair stylists contracted COVID-19 but continued to work for 10 days, servicing 139 clients. Because the salon had a universal masking policy, all stylists and 98% of clients were wearing cloth, surgical, or N95 masks during the encounters. None of the clients or other stylists in the salon developed symptoms9,16. Similar accounts are being reported from around the U.S. and the world13,16,58,59, supported by quantitative simulations60 and randomized controlled trials from other diseases7.
There is also recent evidence that masking is effective at state and national levels. In countries where public masking was common before the pandemic (where it was culturally normal for sick people to wear masks in public), COVID-19 had an initial daily growth rate of 10%, versus 18% in countries without such norms10,61,62. Likewise, the COVID-19 growth rate and mortality rate are lower in countries and states that required public masking12,13,63. The relationship between public masking and lower COVID-19 mortality could be due to lower viral loading (how many particles you are exposed to) decreasing the severity of infection63. This suggests that even when masks do not completely stop transmission, they could still save lives. Universal masking was also pivotal to the success of South Korea and Hong Kong, which were able to contain COVID-19 without lockdowns11,15,64.
There is some anecdotal evidence that masking is working in Utah. Since the mask mandate was passed for Salt Lake and Summit Counties on June 27th, the number of new cases in those areas has decreased, while the number of new cases in the rest of the state has increased65. Likewise, the July 10th request by the Church of Jesus Christ of Latter-day Saints for all members to wear masks in public coincides with a flattening and then decrease of COVID-19 cases statewide66.

Are masks dangerous?
Perhaps the most robust demonstration of the safety of public masking is that this practice has been widely used for decades in many countries, especially in Asia 61,62,76 . In these regions, where it is common to wear a mask when sick or when there is an outbreak masking has proven safe among children, adults, and the elderly 11,23 . Likewise, widespread use in the northeastern U.S. has been highly safe 16,59 . This history of widespread use decreases the risk of unexpected side-effects 76 .
Because masks have been used by medical professionals for centuries, there is a large body of scientific evidence about their performance and safety41,50,56,67–69. Several mild and rare side effects have been identified, including skin irritation, headaches, and general discomfort in a minority of users1,21,22,70. However, certain individuals with acute, preexisting conditions, such as COPD and end-stage renal disease can have difficulty breathing when they wear a respirator (N95) for long periods24,71–74. It is also recommended that individuals should not wear a mask if they cannot remove it on their own—for example, children under two, or people who are unconscious—for common sense, comfort, and safety reasons18.
Despite widespread concern on social media and in the news, there is no evidence that masking causes dangerous hypoxia (low oxygen) or hypercapnia (high carbon dioxide) in healthy individuals, even when multiple masks are layered on top of each other22,70,74. In fact, wearing a surgical mask during exercise has been used as a treatment to reduce exercise-induced asthma69.
There are two main concerns about public masking from a public health perspective, both based on studies of other diseases. First, there can be overcompensation or a “false sense of security,” where mask users are less vigilant in following other preventative measures such as physical distancing or hand washing1,25,62,70. Second, if masks are worn improperly, there can be self-contamination, where bacterial or viral particles accumulated on the outside of the mask are transferred to the hands and then potentially to the mouth or eyes41,54,75. In response to the first concern, observations from this pandemic suggest that wearers of masks are actually more likely to take additional precautions than those who don’t wear masks1,5,11,25. To the second point, mask users should wash their hands after removing their mask and wash masks daily (Figure 1). However, the risk of self-contamination is most likely in clinical situations where masks are used to protect the wearers41,75. This is less of a concern in a public masking scenario, where masks are used to contain infection sources. Additionally, it has been pointed out that “if a mask is contaminated at removal, it has (by definition) already protected the wearer from contagious droplets.”59
Perhaps the most robust demonstration of the safety of public masking is that this practice has been widely used for decades in many countries, especially in Asia61,62,76. In these regions, where it is common to wear a mask when sick or when there is an outbreak masking has proven safe among children, adults, and the elderly11,23. Likewise, widespread use in the northeastern U.S. has been highly safe16,59. This history of widespread use decreases the risk of unexpected side-effects76.
What would the economic consequences be of public masking?
The most recent analysis by Goldman Sachs suggests that increasing masking by 25 percentage points from current levels would cut the COVID-19 growth rate by 3-fold and prevent the need for a second round of economic shutdowns 23 . They predict this would result in an economic benefit of approximately $1 trillion. Another study found that 80% of the population wearing cloth masks when in public would be more effective at stopping the virus than a strict lockdown of the whole population 60 . There is nearly universal consensus that masks could be one of the most powerful and cost-effective tools to stop COVID-19 and accelerate the economic recovery 1,5,10,11,16,23 .
Don't take our word for it The research cited in this report comes from independent medical teams from around the world. Having multiple groups investigate the same question and comparing their independent conclusions increases the reliability of the science. To make it easier for you to evaluate the strength of this evidence, we have compiled PDFs of each cited study in this online folder. To get started, here are five of the most definitive scientific studies on public masking and COVID-19:
For general background, here are 4 fact-checked resources: |
Deep Dive:
What kinds of masks are we talking about?
There are three main types of masks each with different purposes. Experts have advised the general public to wear cloth face coverings to slow the spread of COVID-19, in conjunction with hand washing, physical distancing, and other protective measures (Figure 1).
N95 Respirator: An N95 mask (formally called a respirator) has an extremely small pore size that filters out most particles and aerosols. Given the shortage of these devices, it has been recommended that N95 masks should be reserved and set aside for healthcare workers in clinical settings. Because they are fitted to the face and have such a high filtration capacity, these respirators provide protection from outside droplets and particles.
Surgical Masks: Surgical masks provide basic protection for the wearer but are primarily meant to protect others from droplets and particles coming from the wearer (“source control”). They are sometimes referred to as ‘medical masks.’ Some studies show similar performance to N95 respirators for source control67,75.
Cloth Face Coverings: These are the reusable “home-made” masks that we have been recommended to wear when in public. Surprisingly, they have proven as or more effective as surgical masks and even N95 respirators in some circumstances to contain droplets and disperse air6,17,19,20. They should be washed and dried daily, and some sources recommend alternating days between masks (Figure 1). The level of filtration depends on the type of fabric and number of layers (Figure 2), with multi-layer masks of synthetic and natural fibers outperforming bandanas and neck gaiters, which provide very poor filtration6,20,49,52,53. However, several research groups have pointed out that because the blocking of jets of air and trapping of droplets is the purpose of masks in this pandemic, the most important consideration is comfort, which will increase likelihood of wearing the mask in different environments and reduce adjustments and touching of the mask5,10,59.
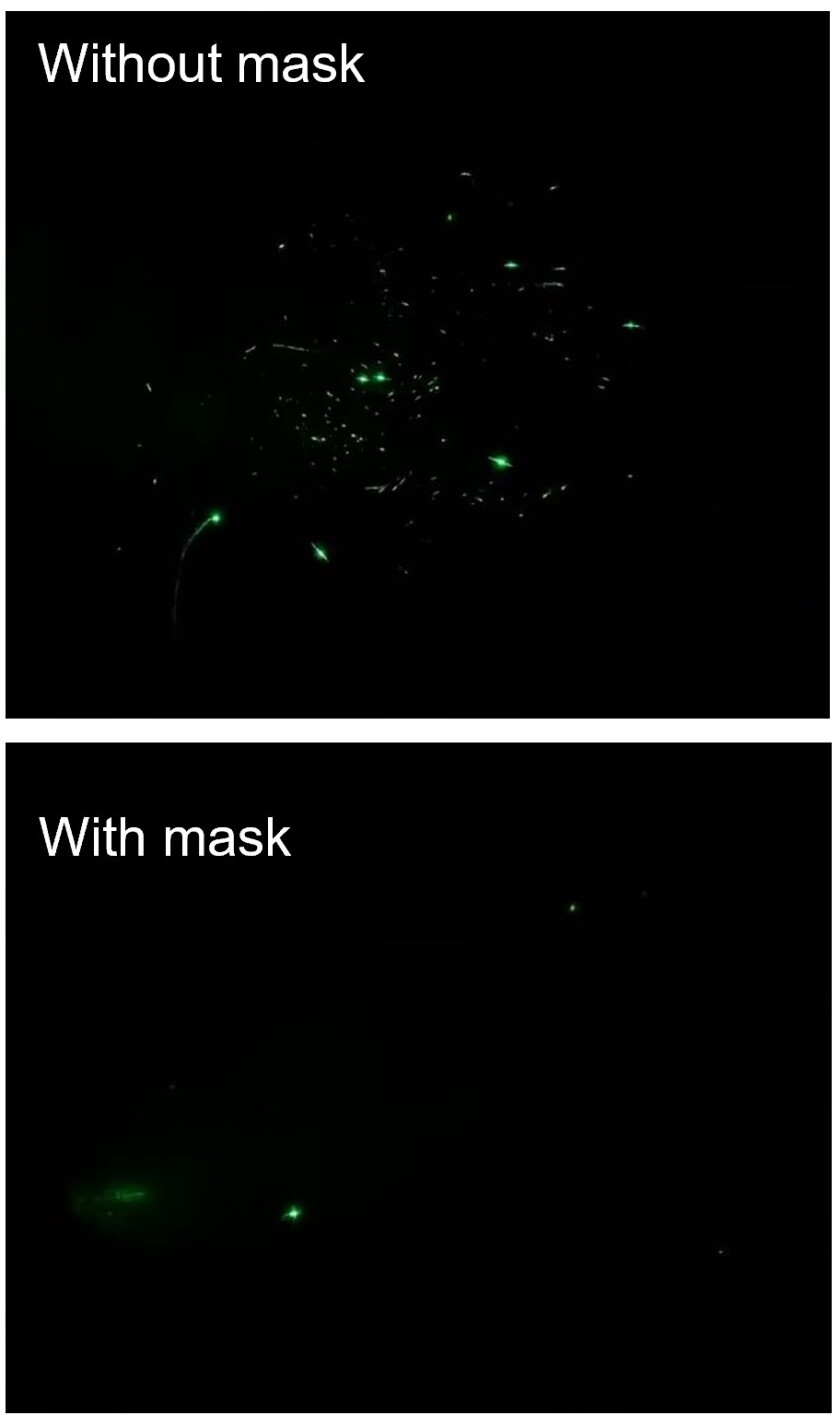
The most recent studies have shown that even a basic covering is quite effective at limiting the spread of infectious respiratory droplets from speaking or coughing (see Figure 3) 6,17,78 . Research measuring the number of droplets from the mouth of someone speaking with and without a mask shows that although cloth coverings certainly aren’t foolproof, they prevent most particles from traveling long distances where they could potentially infect others 6,78 . Multi-layer masks can prevent the spread of more than 90% of respiratory droplets—similar in source control to surgical and N95 masks (Figure 2) 6,20 . Other research has also discovered serious differences in filtration of COVID-19 sized droplets between N95, surgical, and cloth masks. This research also found that the most important thing while wearing a mask is to have a proper fit. Even N95 respirators filtered less than 50% of particles when worn with gaps 49 .

Because of the unparalleled nature of a pandemic in recent history, it was initially difficult to obtain research on the effectiveness of different mask types in public spaces. However, recent studies have shown decreased cases of COVID-19 in areas where masks and social distancing are mandated, and experts say that the efficacy of these mandates will only increase over time13,14,23,77.
The most recent studies have shown that even a basic covering is quite effective at limiting the spread of infectious respiratory droplets from speaking or coughing (see Figure 3)6,17,78. Research measuring the number of droplets from the mouth of someone speaking with and without a mask shows that although cloth coverings certainly aren’t foolproof, they prevent most particles from traveling long distances where they could potentially infect others6,78. Multi-layer masks can prevent the spread of more than 90% of respiratory droplets—similar in source control to surgical and N95 masks (Figure 2)6,20. Other research has also discovered serious differences in filtration of COVID-19 sized droplets between N95, surgical, and cloth masks. This research also found that the most important thing while wearing a mask is to have a proper fit. Even N95 respirators filtered less than 50% of particles when worn with gaps49.
Face coverings in past pandemics:
Since the late 19th century, facemasks have been used in efforts to prevent the spread of infectious diseases. The first studies began using masks to create a sterile surgical environment. By 1920, surgical masks began to be implemented in many hospitals, although they were slow to catch on because surgeons found them to be annoying and generally preferred to not speak while operating76. It wasn’t until the 1960s that masks became widespread in hospitals in the United States. Since then, multiple types of research have been conducted to evaluate how much masks can help, including laboratory tests, “natural experiments” where researchers compare effectiveness of different policies, and computer simulations based on what we know about transmission dynamics and the pathology of COVID-191,5,76.
During the 1918 influenza pandemic, many western cities (including San Francisco, Phoenix, Seattle, and Juneau) tried to mandate facemasks by law. At that time, most Americans did not understand why they needed to wear masks, and they resisted what they perceived as an unnecessary irritant. “The primary purpose of wearing a mask is not to prevent a healthy person from getting sick, but rather to prevent people already infected from contaminating others through casual contact”79. Unfortunately, the 1918 pandemic took the lives of 675,000 Americans, and another 50 million worldwide80. As the United States approaches 140,000 deaths from COVID-19, we should consider all the available evidence on this subject, including context from past pandemics.
COVID-19 and Back to School Efforts:
We have now completed a detailed report on school reopenings during the pandemic, which is accessible here48. We invite you to consult the report directly, but for convenience, we have pasted the executive summary below.
- Children (0-10 years old) and adolescents (11-18) are not immune to COVID-19, though the disease is usually less severe and less easily transmitted by children81–87. Children may be one-third to one-half as susceptible to COVID-19 as middle-aged adults, though adolescents show intermediate to near-adult susceptibility and transmission81,88,89. Transmission by children appears to account for a small minority of overall community and household cases (likely no more than 5 to 10%)82,90–92.
- Evidence on teachers’ risk of infection in school reopenings is limited. Risk of infection may vary based on the school type (lower in elementary, higher in junior high and high school), though this is not well established93–96. Adult to adult contacts within schools may be the greatest risk for teachers97. Protective measures are needed because 1 in 4 teachers is in a high-risk category for COVID-1998.
- Many countries have reopened primary and secondary schools with safe outcomes for students and teachers93,97,99,100. Some outbreaks have occurred, particularly associated with high schools94–96. Factors increasing likelihood of success seem to include: low community spread, preventive measures at school (social distancing, masking, handwashing), rapid testing, contact-tracing, and cohorting101,102.
- No countries have attempted to reopen schools with the level of community spread that the U.S. is currently experiencing. Daily cases in countries that have reopened successfully are typically below 20 per million people100. That number is currently 199 for the U.S. and 120 for Utah65. Early reports from U.S. districts that have reopened suggest frequent exposures , highlighting how reducing community spread should be paramount.
- There are substantial risks and costs associated with not reopening schools, especially for primary and secondary school children, including decreased psychological wellbeing, social development, educational progress, nutrition, and safety103–111. While risks can be dependent on or mitigated by family circumstances for some, many children are highly vulnerable to harm from full school shutdowns112,113.
- Safe reopenings cannot be achieved by interventions at school alone. In-school protective measures must be implemented along with family actions and community support to lower student, teacher, and community infection rates99,101,102,114–116.
- Observational and modeling studies suggest that risk of outbreaks is very high in colleges and universities117–120. This is due to residential and nonresidential student interactions and high transmission among young adults. Widespread and rapid testing, a large quarantine capacity, and a sustained level of vigilance will be needed before campuses can be safely reopened for in-person instruction, even with mask-wearing and social distancing practices in place for classrooms.
In-depth analysis of health risks associated with masking:
Certain health conditions and statuses preclude or increase the risk of wearing face coverings121. Young children under the age of 2 and those who have trouble breathing, due to chronic respiratory conditions or acute or end-stage illness should not wear masks24,73,74,122. Masks are not appropriate for those who are unconscious or otherwise incapable of donning and doffing their own mask. Increased caution should be used when considering masking for individuals with physical, intellectual, or developmental disabilities, such as those of the deaf/hard of hearing community who rely on lip reading to communicate. Lastly, there is little research on the use of masks during exercise, though the World Health Organization recommends against it69,123–125.
As with all medical interventions, there are several documented side effects of wearing a mask. Face masks can cause discomfort, and wearing a mask can direct exhaled breath into the eyes, leading to general irritation and potentially touching the face, which is a danger to transmission and infection70. Wearing a mask in itself can be a reminder to not touch your face, but if they’re adjusted or removed frequently, this may negate the protective benefits against transmission and infection126–128. One study showed that masks were associated with headaches, vague discomfort, and acne, although the headaches were significantly associated with pre-existing headaches21.
Some of the main arguments against masks involve fear of hypoxia and hypercapnia—a lower availability of oxygen and an overabundance of carbon dioxide caused by wearing masks. Professionals, cited in media and press publications, and national and international public health organizations concur that it is highly unlikely for either hypoxia or hypercapnia to occur while wearing a mask15,71,72,122,123,129–131. The only cases where this has been documented to occur are with the use of N95 respirators by medical patients with acute, preexisting conditions, such as AECOPD and end-stage renal disease24,71–73. There are several studies that are widely cited on social media that misinterpret the medical evidence about masks. For example, a small trial of surgical masks among surgeons showed a slight decrease in blood oxygen132. The levels stayed within a healthy range and the authors conclude that the deoxygenation may have been due to the stress of performing surgery rather than the masks.132 Similarly, the studies we cite above about how serious disease can prevent some individuals from safely wearing a mask24,71–73, are often referenced as evidence for why masks are not safe for healthy individuals. The current literature and industry practices indicate that there is very minimal risk of hypoxia and hypercapnia when wearing N95 respirators, and even when a surgical mask is layered on top there appears to be no physiological burden or significant change in oxygen or carbon dioxide levels22,59. There is no evidence that cloth masks, which are looser fit and not sealed, would cause such conditions.
One significant risk of wearing masks lies in overcompensation, also described as the “football-helmet effect.” The concept is that the safety provided by a mask can give a false sense of security, leading to greater disregard of other protective measures. For example, cloth masks primarily provide source control rather than external protection (“my mask protects you, your mask protects me”), though some level of external protection appears likely depending on the fabric and way the mask is worn41,70,126,133. The fear is that someone wearing a mask might be more likely to engage in risky behaviors and therefore put themselves and others at higher risk of infection134. Furthermore, if masks are not worn or cleaned properly, they can result in “self-contamination”18, as discussed previously. While there is no evidence that masks cause fungal or bacterial infections130, the more humid habitat created by a mask may allow SARS-CoV-2 to remain active and possibly lead to the defeat of innate immunity and subsequent infection and transmission70.
In past situations with less virulent diseases and lower levels of community spread, experts expressed caution when extending the successes of mask-wearing to large interpersonal contexts such as schools or healthcare settings41,54,135. They emphasized that other preventative measures such as physical distancing, washing hands, and staying home would be more effective than purely relying on masks136. In the current pandemic, the consensus is growing that public masking should be used in combination with other efforts rather than not at all1,5,7,10,126,133,136. Even the cautious and consensus-driven World Health Organization, which initially recommended against masks, now encourages their use in areas of widespread COVID-19 transmission137, in light of new information on the disease and the results of large-scale comparative studies135.
Frequently asked questions (FAQs):
1. How did you select the papers you included?
We generated an initial list of studies using Google Scholar and Web of Science. We focused this initial search on studies specifically dealing with COVID-19 and masks. As we read those papers, we added pertinent studies they cited to our list. Additionally, we considered about a dozen studies that concerned individuals sent us. These studies were mostly about the safety of masks. Our goal was to provide a non-technical summary for those interested in this topic. Because the medical literature on COVID-19 is so large, we cite many studies that are reviews, summaries, and commentaries on the state of the literature. While we also read many specific primary research articles, we favored citations of reviews and summaries to encourage readers to interact with the peer-reviewed holistic assessment of the state of scientific understanding. These synthesis papers are often more reliable and robust than any individual study upon which they draw138. They also avoid the "single-study syndrome," where one study is interpreted without context from other work. Science is a joint venture and only reliable when the result is repeatable and falsifiable.
2. How did you ensure you weren’t getting a biased sample of studies?
We considered all the scientific studies on masks and COVID-19 that we could find, including about a dozen sent to us by individuals who do not support masking. We continue to consider all studies that are sent, so if we missed a particularly pertinent piece on COVID-19 and masks, please send it along (but please read FAQ #4 before sending unrelated studies). Likewise, if you see an error or point of confusion in the report, please let us know and we will update if we find there is an error. This has happened several times already, mainly with typos, but also with two important mistakes: 1. In the viral transmission section, we initially wrote “COVID-19 viruses” when the study in question was actually about coronaviruses generally, and 2. Our initial description of the most recent WHO recommendations were confusing. At the top of the report, we mention the “last updated on” date, so you can know when the last change was made.
3. Why do you cite some non-scientific sources such as news articles and government reports?
We cited a few of these articles for context to provide an idea of what the larger conversation is outside of science. In one section (the deep dive on mask safety), we cite some of these news reports because they have quotes from legitimate medical experts. We mention that we are citing media sources in that section to make sure people know what we are basing our interpretation on.
4. What about this or that study that was done on another disease?
There is a huge amount of research on other diseases, including several on the effectiveness of public masking in stopping those diseases (though fewer than we expected)7,40,41,54. We cite some of this research in our report to provide context. For example, it’s helpful to know that public masking was widely considered ineffective before the COVID-19 pandemic based on studies done with other diseases in very different contexts. This explains why many medical experts and agencies recommend against mass masking initially—that was the state of the available science in December 2019 and January 2020.
For our report, we focus heavily on the COVID-19-specific studies for one very important reason: COVID-19 is the disease causing this pandemic. Findings from previous outbreaks and community studies are helpful as a starting place, especially in the absence of more directly pertinent evidence. However, the pathology of each disease and the societal dynamics of each outbreak are different. Naively applying findings about influenza and masks in normal times to COVID-19 during a global pandemic is problematic, to say the least. As we evaluated the evidence from multiple studies, we gave more weight to those that dealt specifically with the current outbreak, while still considering the other studies for context.
One specific study is worth mentioning here, because of how often it is brought up in discussions of masks: MacIntyre and others 2015, "Facemasks for the prevention of infection in healthcare and community settings."40 This study is often brought up as evidence that masks (especially cloth masks) don't work, and that they might actually cause harm (increase risk of infection). On first read of the abstract, it is easy to get this impression. However, this is a completely incorrect interpretation of this research for several reasons. First, the study is on different diseases in different conditions (see last two paragraphs). Second, the study tested the effectiveness of masks at protecting the wearer (in this case healthcare workers), rather than source control, which is the primary purpose of masks in the COVID-19 pandemic. Third, the study did not have a "no mask" control, so they have no way of comparing cloth mask with no mask. The authors make this clear in the "Strengths and limitations" section of their paper, which appears adjacent to the abstract when you download the PDF. Importantly, the same research group did a study the following year on the effectiveness of masks at reducing infection when worn by sick individuals41. They found that masks likely reduced infection, though they acknowledge that they didn't have enough participants to strongly conclude anything. Since the COVID-19 pandemic, this research group has done a systematic review of the effectiveness of masks7, including their 2015 study. They conclude:
“community mask use by well people could be beneficial, particularly for COVID-19, where transmission may be pre-symptomatic. The studies of masks as source control also suggest a benefit, and may be important during the COVID-19 pandemic in universal community face mask use as well as in health care settings.”
5. Why don’t you cite this or that specific study?
There are thousands of papers on COVID-19, which is a scientific achievement on its own. I salute the researchers and organizations that have, often at great expense, changed their research programs to address this important challenge. However, this means that we cannot cite every study on COVID. See the previous FAQs for info on how we decided what to focus on and what to cite.
6. Why do you claim there are controlled experiments when there haven’t been any randomized controlled trials of public masking?
One of the most common arguments made against masking is that there aren’t any randomized controlled trials (RCTs) showing effectiveness of public masking. This is not true. A very recent systematic review by Macintyre and Chughtai7 of public masking studies (including many RCTs) concluded that masks are effective at slowing the spread of many respiratory diseases. Additional RCTs on this subject are coming out frequently55. However, there are not, to our knowledge, any COVID-19 specific RCTs yet published. This deserves some context.
RCTs are powerful tools that can—when done correctly—quantify the effectiveness of a drug or other intervention. They are often described as the gold standard for establishing cause and effect and are usually required before high-risk changes in medical practice are implemented (for example introducing a new medication). RCTs also take time and ethically require that the trial doesn’t cause undue risk or harm to the participants. In the context of a global pandemic, it is not surprising that there are not yet RCTs on COVID-19 and public masking. Indeed, concern over the lack of RCTs sparked a fruitful discussion in the medical community (mainly in March and April), as it should have, about whether to change recommendations without RCTs. Check out this paper by Greenhalgh and colleagues1 from April for a snapshot of what was being discussed at that point.
As this discussion played out in the medical community, other types of evidence started becoming available, including:
- Longitudinal studies quantifying infection rates and death rates after implementation of masking in different settings
- Comparative studies measuring outcomes in different regions and countries
- Case studies of specific events where the virus was or was not transmitted
- Large-scale studies on the pathology (transmission dynamics, contagiousness, symptoms, etc.) of COVID-19
- Laboratory studies quantifying the effectiveness of masks in filtering, muffling, and containing particles and droplets
The first two types of studies often cannot definitively establish the specific cause of the outcome; for example, how much was the masking itself versus the psychological reminder to respect greater physical distance that resulted in the decrease in death? However, they are extremely powerful (and often more robust because they can involve many more people than even the largest RCT) at assessing overall outcome of an intervention. The third kind of study can’t provide definitive evidence of the generality of an intervention (e.g. will masks always protect people getting their hair done by an infected hair dresser?), but in the absence of more controlled studies, these case studies are indispensable as metrics of real-world performance and outcomes. The fourth and fifth kinds of studies complement the others by establishing specifics of how the disease works and first-order estimates of potential effectiveness of interventions (in this case masking).
Given the mounting evidence, most medical experts and public health entities updated their recommendations early this year. Given the high likelihood of benefit and the extremely low risk of the intervention (there is abundant evidence that mask wearing is exceedingly safe for healthy individuals), recommending public masking was determined to be the only ethical course of action. While most papers we read continue to call for RCTs in their conclusions or discussion, they also recognized that such results could still be months or years out. Some papers have also pointed out that given the strength of the evidence, an RCT on public masking may no longer be ethical because asking people to not wear masks in areas of COVID-19 would knowingly endanger participants.
Because our report is meant for a general audience, we classified studies as controlled or observational. We used controlled to refer to any study with a manipulation (for example, implementation of healthcare worker and then patient masking in the Massachusetts study, or lab experiments on mask filtration of droplets and viral particles). We used observational to refer to studies that compare groups or outcomes without a targeted intervention. We recognize this division is imperfect, but after discussion, we decided it was a clearer distinction than observational and manipulative, the more common scientific terms.
7. Were you trying to prove something with this study? Aren't you biased?
Our only purpose in performing this research was to make more of the science available to the public. Here is the email Dr. Abbott sent to his lab group on July 14th, when he initiated the project:
Dear lab group,
Just reaching out to see if any of you might be interested in contributing to a one or two page report on efficacy and risks of wearing masks? Maybe it's just my social media feed, which is dominated by moms and dads, but this appears to be a hot topic right now. As there is very little trust in currently available summaries, I think a succinct and carefully nonpoliticial mini-review could do a lot of good. I don't know if it would be publishable in a peer-reviewed journal (depends on how much we want to put into it), but we could easily self publish on the lab website and do a press release.
To the question of bias, yes, like all humans, we are. Our beliefs and values influence how we see the world around us. We discussed this as a group of authors and worked hard to provide a fair summary of the literature. Staying neutral was helped by the variety of political views and backgrounds among the co-authors. We take scientific integrity extremely seriously, plus I believe that we have a God-given responsibility to be honest. We recognize there are inevitable gaps and room for improvement, but we have done my best to accurately represent the scientific literature.
Especially during these politically charged times, all of us need to be extra vigilant and responsible about what we share and say. Whether it is this report or anything else, please read the article before reposting and interpreting it on social media. It’s a matter of basic honesty and integrity. Plus, what we say and share has serious consequences in the real world.
REFERENCES
- Greenhalgh, T., Schmid, M. B., Czypionka, T., Bassler, D. & Gruer, L. Face masks for the public during the covid-19 crisis. BMJ 369, (2020).
- Wang, G., Zhang, Y., Zhao, J., Zhang, J. & Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet 395, 945–947 (2020).
- Mahase, E. Covid-19: What is the evidence for cloth masks? BMJ 369, (2020).
- Schünemann, H. J. et al. Use of facemasks during the COVID-19 pandemic. The Lancet Respiratory Medicine 0, (2020).
- Howard, J. et al. Face Masks Against COVID-19: An Evidence Review. In Review (2020) doi:10.20944/preprints202004.0203.v1.
- Fischer, E. P. et al. Low-cost measurement of facemask efficacy for filtering expelled droplets during speech. Science Advances eabd3083 (2020) doi:10.1126/sciadv.abd3083.
- MacIntyre, C. R. & Chughtai, A. A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud 108, 103629 (2020).
- Wang, X., Ferro, E. G., Zhou, G., Hashimoto, D. & Bhatt, D. L. Association Between Universal Masking in a Health Care System and SARS-CoV-2 Positivity Among Health Care Workers. JAMA (2020) doi:10.1001/jama.2020.12897.
- Hendrix, M. J. Absence of Apparent Transmission of SARS-CoV-2 from Two Stylists After Exposure at a Hair Salon with a Universal Face Covering Policy — Springfield, Missouri, May 2020. MMWR Morb Mortal Wkly Rep 69, (2020).
- Abaluck, J. et al. The Case for Universal Cloth Mask Adoption and Policies to Increase Supply of Medical Masks for Health Workers. https://papers.ssrn.com/abstract=3567438 (2020) doi:10.2139/ssrn.3567438.
- Tam, V. C., Tam, S. Y., Poon, W. K., Law, H. K. W. & Lee, S. W. A reality check on the use of face masks during the COVID-19 outbreak in Hong Kong. EClinicalMedicine 22, 100356 (2020).
- Kenyon, C. Widespread use of face masks in public may slow the spread of SARS CoV-2: an ecological study. http://medrxiv.org/lookup/doi/10.1101/2020.03.31.20048652 (2020) doi:10.1101/2020.03.31.20048652.
- Lyu, W. & Wehby, G. L. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US: Study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health Affairs 10.1377/hlthaff (2020) doi:10.1377/hlthaff.2020.00818.
- Li, T., Liu, Y., Li, M., Qian, X. & Dai, S. Y. Mask or no mask for COVID-19: A public health and market study. PLOS ONE 15, e0237691 (2020).
- Cheng, K. K., Lam, T. H. & Leung, C. C. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. The Lancet 0, (2020).
- Brooks, J. T., Butler, J. C. & Redfield, R. R. Universal Masking to Prevent SARS-CoV-2 Transmission—The Time Is Now. JAMA (2020) doi:10.1001/jama.2020.13107.
- Anfinrud, P., Stadnytskyi, V., Bax, C. E. & Bax, A. Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. New England Journal of Medicine 382, 2061–2063 (2020).
- Desai, A. N. & Aronoff, D. M. Masks and Coronavirus Disease 2019 (COVID-19). JAMA 323, 2103–2103 (2020).
- Verma, S., Dhanak, M. & Frankenfield, J. Visualizing the effectiveness of face masks in obstructing respiratory jets. Physics of Fluids 32, 061708 (2020).
- Aydin, O. et al. Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study. Extreme Mech Lett (2020) doi:10.1016/j.eml.2020.100924.
- Lim, E. C. H. et al. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurologica Scandinavica 113, 199–202 (2006).
- Roberge, R. J., Coca, A., Williams, W. J., Palmiero, A. J. & Powell, J. B. Surgical mask placement over N95 filtering facepiece respirators: Physiological effects on healthcare workers. Respirology 15, 516–521 (2010).
- Goldman Sachs Research. Face Masks and GDP. https://www.goldmansachs.com/insights/pages/face-masks-and-gdp.html (2020).
- Kao, T.-W. et al. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J. Formos. Med. Assoc. 103, 624–628 (2004).
- Mantzari, E., Rubin, G. J. & Marteau, T. M. Is risk compensation threatening public health in the covid-19 pandemic? BMJ 370, (2020).
- Kretzschmar, M. E. et al. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. The Lancet Public Health 0, (2020).
- Cohen, J. A WHO-led mission may investigate the pandemic’s origin. Here are the key questions to ask. https://www.sciencemag.org/news/2020/07/who-led-mission-may-investigate-pandemic-s-origin-here-are-key-questions-ask (2020).
- Plapp, F. The COVID-19 Pandemic: A Summary. The Pathologist 14 (2020).
- Rajgor, D. D., Lee, M. H., Archuleta, S., Bagdasarian, N. & Quek, S. C. The many estimates of the COVID-19 case fatality rate. The Lancet Infectious Diseases 20, 776–777 (2020).
- Wu, Z. & McGoogan, J. M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 323, 1239–1242 (2020).
- Xu, Z. et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. The Lancet Respiratory Medicine 8, 420–422 (2020).
- Baud, D. et al. Real estimates of mortality following COVID-19 infection. The Lancet Infectious Diseases 20, 773 (2020).
- Liu Peter P., Blet Alice, Smyth David & Li Hongliang. The Science Underlying COVID-19. Circulation 142, 68–78 (2020).
- D Sleator, R., Darby, S., Giltinan, A. & Smith, N. COVID-19: in the absence of vaccination – ‘mask-the-nation’. Future Microbiology fmb-2020-0112 (2020) doi:10.2217/fmb-2020-0112.
- Contini, D. & Costabile, F. Does Air Pollution Influence COVID-19 Outbreaks? Atmosphere 11, 377 (2020).
- Wu, X., Nethery, R. C., Sabath, B. M., Braun, D. & Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. http://medrxiv.org/lookup/doi/10.1101/2020.04.05.20054502 (2020) doi:10.1101/2020.04.05.20054502.
- Qian, G. et al. COVID-19 Transmission Within a Family Cluster by Presymptomatic Carriers in China. Clinical Infectious Diseases ciaa316 (2020) doi:10.1093/cid/ciaa316.
- van Doremalen, N. et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 382, 1564–1567 (2020).
- Bourouiba, L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19. JAMA 323, 1837–1838 (2020).
- MacIntyre, C. R. & Chughtai, A. A. Facemasks for the prevention of infection in healthcare and community settings. BMJ 350, h694 (2015).
- MacIntyre, C. R. et al. Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open 6, e012330 (2016).
- Peng, Y. & Zhou, Y. Is novel coronavirus disease (COVID‐19) transmitted through conjunctiva? J Med Virol (2020) doi:10.1002/jmv.25753.
- Wei, W. E. et al. Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 411–415 (2020).
- Eikenberry, S. E. et al. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infectious Disease Modelling 5, 293–308 (2020).
- Nishiura, H. et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). medRxiv 2020.02.03.20020248 (2020) doi:10.1101/2020.02.03.20020248.
- Bai, Y. et al. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 323, 1406–1407 (2020).
- Ganyani, T. et al. Estimating the generation interval for coronavirus disease (COVID-19) based on symptom onset data, March 2020. Euro Surveill 25, (2020).
- Abbott, B. W. et al. Making sense of the research on COVID-19 and school reopenings. 22 http://rgdoi.net/10.13140/RG.2.2.24052.17285 (2020).
- Konda, A. et al. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano 14, 6339–6347 (2020).
- Leung, N. H. L. et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine 26, 676–680 (2020).
- Mueller, A. & Fernandez, L. Assessment of Fabric Masks as Alternatives to Standard Surgical Masks in Terms of Particle Filtration Efficiency. 8 (2020).
- Mueller, A. V., Eden, M. J., Oakes, J. M., Bellini, C. & Fernandez, L. A. Quantitative Method for Comparative Assessment of Particle Removal Efficiency of Fabric Masks as Alternatives to Standard Surgical Masks for PPE. Matter (2020) doi:10.1016/j.matt.2020.07.006.
- Rengasamy, S., Eimer, B. & Shaffer, R. E. Simple Respiratory Protection—Evaluation of the Filtration Performance of Cloth Masks and Common Fabric Materials Against 20–1000 nm Size Particles. Ann Occup Hyg 54, 789–798 (2010).
- Chughtai, A. A., Seale, H. & MacIntyre, C. R. Use of cloth masks in the practice of infection control – evidence and policy gaps. Int. j. infect. control 9, (2013).
- Dugré, N. et al. Masks for prevention of viral respiratory infections among health care workers and the public. Can Fam Physician 66, 509–517 (2020).
- Oberg, T. & Brosseau, L. M. Surgical mask filter and fit performance. American Journal of Infection Control 36, 276–282 (2008).
- Chu, D. K. et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet 395, 1973–1987 (2020).
- Liu, X. & Zhang, S. COVID-19: Face masks and human-to-human transmission. Influenza and Other Respiratory Viruses 14, 472–473 (2020).
- Javid, B., Weekes, M. P. & Matheson, N. J. Covid-19: should the public wear face masks? BMJ 369, (2020).
- Kai, D., Goldstein, G.-P., Morgunov, A., Nangalia, V. & Rotkirch, A. Universal Masking is Urgent in the COVID-19 Pandemic: SEIR and Agent Based Models, Empirical Validation, Policy Recommendations. arXiv:2004.13553 [physics, q-bio] (2020).
- Longrich, N. R. & Sheppard, S. K. Public use of face masks to control the coronavirus (SARS-Cov-2) pandemic: a review of theory and evidence. In Review 17 (2020).
- Royal Society. Face Masks for the General Public. http://rs-delve.github.io/reports/2020/05/04/face-masks-for-the-general-public.html (2020).
- Leffler, C. T., Ing, E., McKeown, C. A., Pratt, D. & Grzybowski, A. Final Country-wide Mortality from the Novel Coronavirus (COVID-19) Pandemic and Notes Regarding Mask Usage by the Public. In Review 14 (2020).
- Cowling, B. J. et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. The Lancet Public Health 5, e279–e288 (2020).
- Utah Department of Health. Utah Case Counts | coronavirus. https://coronavirus.utah.gov/case-counts/ (2020).
- Saal, M. LDS church asks members in Utah to wear masks to prevent COVID-19 spread | Faith | heraldextra.com. Daily Herald (2020).
- Long, Y. et al. Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis. Journal of Evidence-Based Medicine 13, 93–101 (2020).
- Atkinson, J. et al. Respiratory droplets. (World Health Organization, 2009).
- Brenner, A. M., Weiser, P. C., Krogh, L. A. & Loren, M. L. Effectiveness of a Portable Face Mask in Attenuating Exercise-Induced Asthma. JAMA 244, 2196–2198 (1980).
- Lazzarino, A. I., Steptoe, A., Hamer, M. & Michie, S. Covid-19: important potential side effects of wearing face masks that we should bear in mind. (2020).
- From the Frontlines: The Truth About Masks and COVID-19 | American Lung Association. https://www.lung.org/blog/covid-masks.
- Killer COVID-19 Masks? The Truth About Trapped Carbon Dioxide | Hartford HealthCare. https://hartfordhealthcare.org/about-us/news-press/news-detail?articleid=26712&publicId=395.
- Risk and impact of using mask on COPD patients with acute exacerbation during the COVID-19 outbreak: a retrospective study. (2020) doi:10.21203/rs.3.rs-39747/v1.
- Matuschek, C. et al. Face masks: benefits and risks during the COVID-19 crisis. European Journal of Medical Research 25, 32 (2020).
- Abd-Elsayed, A. & Karri, J. Utility of Substandard Face Mask Options for Health Care Workers During the COVID-19 Pandemic. Anesthesia & Analgesia 131, 4–6 (2020).
- Matuschek, C. et al. The history and value of face masks. European Journal of Medical Research 25, 23 (2020).
- Gostin, L. O., Cohen, I. G. & Koplan, J. P. Universal Masking in the United States: The Role of Mandates, Health Education, and the CDC. JAMA (2020) doi:10.1001/jama.2020.15271.
- Fisman, D. N., Greer, A. L. & Tuite, A. R. Bidirectional impact of imperfect mask use on reproduction number of COVID-19: A next generation matrix approach. Infectious Disease Modelling 5, 405–408 (2020).
- Ewing, E. T. Flu Masks Failed In 1918, But We Need Them Now | Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200508.769108/full/.
- 1918 Pandemic (H1N1 virus) | Pandemic Influenza (Flu) | CDC. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html (2020).
- Dattner, I. et al. The role of children in the spread of COVID-19: Using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. medRxiv 2020.06.03.20121145 (2020) doi:10.1101/2020.06.03.20121145.
- Lee, B. & Raszka, W. V. COVID-19 Transmission and Children: The Child Is Not to Blame. Pediatrics 146, (2020).
- Ludvigsson, J. F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica 109, 1088–1095 (2020).
- Ludvigsson, J. F. Children are unlikely to be the main drivers of the COVID-19 pandemic - A systematic review. Acta Paediatr. 109, 1525–1530 (2020).
- Munro, A. P. S. & Faust, S. N. Children are not COVID-19 super spreaders: time to go back to school. Archives of Disease in Childhood 105, 618–619 (2020).
- Zhen-Dong, Y. et al. Clinical and transmission dynamics characteristics of 406 children with coronavirus disease 2019 in China: A review. Journal of Infection 81, e11–e15 (2020).
- Zhu, Y. et al. Children are unlikely to have been the primary source of household SARS-CoV-2 infections. medRxiv 2020.03.26.20044826 (2020) doi:10.1101/2020.03.26.20044826.
- Davies, N. G. et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nature Medicine 1–7 (2020) doi:10.1038/s41591-020-0962-9.
- Park, Y. J. et al. Early Release - Contact Tracing during Coronavirus Disease Outbreak, South Korea, 2020. Emerging Infectious Diseases Volume 26, (2020).
- Posfay-Barbe, K. M. et al. COVID-19 in Children and the Dynamics of Infection in Families. Pediatrics 146, (2020).
- Li, X. et al. The role of children in transmission of SARS-CoV-2: A rapid review. Journal of Global Health 10, 011101 (2020).
- Walger, P. et al. Children and adolescents in the CoVid-19 pandemic: Schools and daycare centers are to be opened again without restrictions. The protection of teachers, educators, carers and parents and the general hygiene rules do not conflict with this. GMS Hyg Infect Control 15, Doc11 (2020).
- Fontanet, A. et al. SARS-CoV-2 infection in primary schools in northern France: A retrospective cohort study in an area of high transmission. medRxiv 2020.06.25.20140178 (2020) doi:10.1101/2020.06.25.20140178.
- Fontanet, A. et al. Cluster of COVID-19 in northern France: A retrospective closed cohort study. medRxiv 2020.04.18.20071134 (2020) doi:10.1101/2020.04.18.20071134.
- Stein-Zamir, C. et al. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Eurosurveillance 25, 2001352 (2020).
- Stage, H. B. et al. Shut and re-open: the role of schools in the spread of COVID-19 in Europe. medRxiv 2020.06.24.20139634 (2020) doi:10.1101/2020.06.24.20139634.
- Macartney, K. et al. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. The Lancet Child & Adolescent Health 0, (2020).
- Claxton, G., Kamal, R. & 2020. How Many Teachers Are at Risk of Serious Illness If Infected with Coronavirus? KFF https://www.kff.org/coronavirus-covid-19/issue-brief/how-many-teachers-are-at-risk-of-serious-illness-if-infected-with-coronavirus/ (2020).
- Couzin-Frankel, J., Vogel, G. & Weil, M. School openings across globe suggest ways to keep coronavirus at bay, despite outbreaks. Science (2020).
- Michaud, J. & Kates, J. What Do We Know About Children and Coronavirus Transmission? KFF https://www.kff.org/coronavirus-covid-19/issue-brief/what-do-we-know-about-children-and-coronavirus-transmission/ (2020).
- CDC. Preparing K-12 School Administrators for a Safe Return to School in Fall 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/prepare-safe-return.html (2020).
- ECDC. COVID-19 in children and the role of school settings in COVID-19 transmission. https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission (2020).
- American Academy of Pediatrics (AAP). COVID-19 Planning Considerations: Guidance for School Re-entry. http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/ (2020).
- Baron, E. J., Goldstein, E. G. & Wallace, C. T. Suffering in Silence: How COVID-19 School Closures Inhibit the Reporting of Child Maltreatment. Journal of Public Economics (2020) doi:10.2139/ssrn.3601399.
- Christakis, D. A. School Reopening—The Pandemic Issue That Is Not Getting Its Due. JAMA Pediatr (2020) doi:10.1001/jamapediatrics.2020.2068.
- Crawley, E. et al. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatrics Open 4, e000701 (2020).
- Dibner, K. A., Schweingruber, H. A. & Christakis, D. A. Reopening K-12 Schools During the COVID-19 Pandemic: A Report From the National Academies of Sciences, Engineering, and Medicine. JAMA (2020) doi:10.1001/jama.2020.14745.
- Lancker, W. V. & Parolin, Z. COVID-19, school closures, and child poverty: a social crisis in the making. The Lancet Public Health 5, e243–e244 (2020).
- Marchetti, F. & Tamburlini, G. Time to go back to school: several good reasons beyond low infection risk. BMJ 370, (2020).
- Rundle, A. G., Park, Y., Herbstman, J. B., Kinsey, E. W. & Wang, Y. C. COVID-19–Related School Closings and Risk of Weight Gain Among Children. Obesity 28, 1008–1009 (2020).
- Sharfstein, J. M. & Morphew, C. C. The Urgency and Challenge of Opening K-12 Schools in the Fall of 2020. JAMA 324, 133–134 (2020).
- Armitage, R. & Nellums, L. B. Considering inequalities in the school closure response to COVID-19. The Lancet Global Health 8, e644 (2020).
- Masonbrink, A. R. & Hurley, E. Advocating for Children During the COVID-19 School Closures. Pediatrics (2020) doi:10.1542/peds.2020-1440.
- Utah Department of Health (UDOH). COVID-19 School Manual. https://coronavirus-download.utah.gov/School/COVID-19_School_Manual_FINAL.pdf (2020).
- Kinetic West. Best Practices for Reopening WA Schools. https://www.k12.wa.us/sites/default/files/public/workgroups/Kinetic-West-PPT-June-2-2020-Best-Practices-for-Reopening-WA-Schools.pdf (2020).
- UNICEF. Framework for reopening schools. https://www.unicef.org/media/68366/file/Framework-for-reopening-schools-2020.pdf (2020).
- Gressman, P. T. & Peck, J. R. Simulating COVID-19 in a University Environment. arXiv:2006.03175 [physics, q-bio] (2020).
- Mossa-Basha, M. et al. Policies and Guidelines for COVID-19 Preparedness: Experiences from the University of Washington. Radiology 201326 (2020) doi:10.1148/radiol.2020201326.
- Paltiel, A. D., Zheng, A. & Walensky, R. P. Assessment of SARS-CoV-2 Screening Strategies to Permit the Safe Reopening of College Campuses in the United States. JAMA Netw Open 3, e2016818–e2016818 (2020).
- Wang, C., Cheng, Z., Yue, X.-G. & McAleer, M. Risk Management of COVID-19 by Universities in China. Journal of Risk and Financial Management 13, 36 (2020).
- CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html (2020).
- ‘Frightening’: Doctor debunks claims that wearing a face mask is more harmful than COVID-19. Coronavirus https://www.ctvnews.ca/health/coronavirus/frightening-doctor-debunks-claims-that-wearing-a-face-mask-is-more-harmful-than-covid-19-1.4986734 (2020).
- COVID-19 Mythbusters – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.
- Li, Y. et al. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Arch Occup Environ Health 78, 501–509 (2005).
- Pifarré, F., Zabala, D. D., Grazioli, G. & de Yzaguirre i Maura, I. COVID 19 and mask in sports. Apunts Sports Medicine S2666506920300250 (2020) doi:10.1016/j.apunsm.2020.06.002.
- Tirupathi, R., Bharathidasan, K., Palabindala, V., Salim, S. A. & Al-Tawfiq, J. A. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. 5 Mistakes You May Be Making When Wearing Face Masks. Moffitt Cancer Center https://moffitt.org/endeavor/archive/5-mistakes-you-may-be-making-when-wearing-face-masks/.
- How Not to Touch Your Face. https://www.umms.org:443/coronavirus/what-to-know/symptoms-prevention/not-touch-face.
- Carmichael, J. G. and F. ‘Deadly mask’ claims debunked. BBC News (2020).
- Does wearing a mask pose any health risks? https://medicalxpress.com/news/2020-07-mask-pose-health.html.
- Debunked myths about face masks. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/debunked-myths-about-face-masks.
- Beder, A., Büyükkoçak, Ü., Sabuncuoğlu, H., Keskil, Z. A. & Keskil, S. Preliminary report on surgical mask induced deoxygenation during major surgery. 6 (2008).
- Davies, A. et al. Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic? Disaster med. public health prep. 7, 413–418 (2013).
- Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak. https://www.who.int/publications-detail-redirect/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak.
- To wear or not to wear: WHO’s confusing guidance on masks in the covid-19 pandemic. The BMJ https://blogs.bmj.com/bmj/2020/03/11/whos-confusing-guidance-masks-covid-19-epidemic/ (2020).
- MacIntyre, C. R. et al. Face Mask Use and Control of Respiratory Virus Transmission in Households - Volume 15, Number 2—February 2009 - Emerging Infectious Diseases journal - CDC. doi:10.3201/eid1502.081167.
- Timeline of WHO’s response to COVID-19. https://www.who.int/news-room/detail/29-06-2020-covidtimeline.
- Ioannidis, J. P. A. Why Most Published Research Findings Are False. PLoS Med 2, e124 (2005).